Hemispherotomy = Hemispherotomy? Typology of different functional disconnection procedures1/18/2024 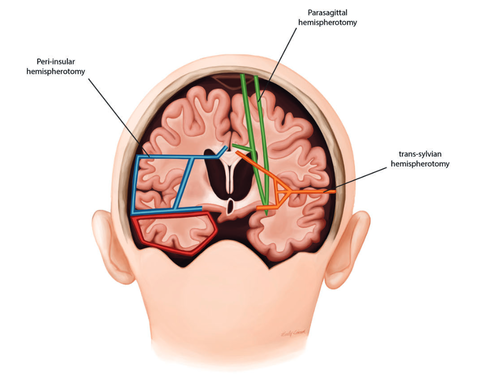 Nurida Boddenberg Hemispherotomy, a medical procedure performed in severe epilepsy cases, has sparked interesting debates surrounding unusual or borderline consciousness. Its outcomes are often associated with an anatomically preserved cerebral hemisphere that is, however, devoid of any functional connection to the rest of the body or the brain. Still, the isolated hemisphere is sometimes physiologically intact and allows for electrophysiological studies (Hawasli 2017), which has provoked (Baynes, Seth, Massimini 2020) to propose the idea of an 'island of awareness' in this context. However, the actual outcome of the hemispheric-resection procedure varies, which could also possibly change and impact how our islands of awareness might look, with implications for the consciousness debate. The objective of this post is to clarify the various procedures that are referred to under the term "hemispherotomy". Figure 1: A schematic representation of some of the common hemispherotomy procedures. Peri-insular hemispherotomy (blue), sometimes additionally in this procedure the temporal lobe (red) is resected. Trans-sylvian hemispherotomy (orange) and parasagittal hemispherotomy (green) Picture from Cohen, A. R (2016): Section VIII: Epilepsy and Functional Disorders. In: Pedriatic Neurosurgery The controlled resection of hemispheres started in the 1920s with the complete removal of one hemisphere – anatomic hemispherectomy (Dandy). However, advances in neurosurgery after the 1970s led to less invasive techniques such as hemidecortication (Ignelzi and Bucy) and functional hemispherectomy (Rasmussen), which prioritize maintaining more anatomical integrity while achieving the desired functional disconnection. Still, much of the cerebral material is removed, which reduced the chances of conscious ongoings in this hemisphere. Then, in the 1990s, a refined set of techniques emerged under the term `hemispherotomy,' aiming to isolate the affected brain hemisphere functionally but with even less tissue removal. This procedure reduced risks like blood loss and infection but raised concerns about incomplete disconnections and the potential need for a second surgery. (See Figure 1 for a comparison of the extent of disconnection) The choice of specific hemispherotomy technique is a critical decision influenced by various factors, such as the tools available, the surgeon's expertise, and the patient's specific pathology, each bearing distinct intricacies that can influence the postoperative structure and affect the likelihood of disconnection. The vertical parasagittal hemispherotomy (Delalande) utilizes a vertical incision near the brain's midline to access the corpus callosum and white matter tracts for disconnection, ideal for cases of cerebral hemispheric atrophy. In contrast, the peri-insular hemispherotomy (Villemure and Daniel) uses a lateral approach to disconnect the affected hemisphere, providing the shortest working corridor and preserving deep structures like the thalamus, midbrain, basal ganglia, cerebral arteries, and cranial nerves. Further, the lateral transsylvian (keyhole) approach (Schramm) is a variation of the peri-insular technique. It navigates through the Sylvian fissure to excise parts of the inner temporal lobe, proceeding with disconnections at the frontal lobe, through the corpus callosum, and extending to the parietal and occipital regions, suited for patients with large cysts between the frontal and temporal lobe. However, both lateral hemispherotomy methods used to lead to quicker seizure recurrence and higher odds of seizure return compared to vertical techniques, possibly due to a less thorough disconnection., which could result in residual sensory input or motor afferences, thereby affecting potential `awareness’ in the isolated hemisphere. Endoscopic hemispherotomy (Chandra and Sood) marks a significant milestone in minimally invasive neurosurgery. This technique employs endoscopic instruments to perform the procedure through smaller openings, aiming to minimize complications (e.g., blood loss) while striving to preserve its efficacy. However, if brain structures lie deep and parallel to the plane of disconnection, they are more prone to be missed, which might lead to persistent or recurrent seizures and less disconnected paths. However, one may note that after hemispherotomy the isolated hemisphere could shrink, especially if certain blood vessels are tied off during the procedure, with long-term results quite similar to those of an anatomical hemispherectomy. In conclusion, while hemispherotomy is a critical intervention for those suffering from severe epilepsy, it also has the potential to offer a unique window into understanding consciousness. By revisiting the initial question, we recognize that hemispherotomy isn't just about disconnecting a dysfunctional hemisphere; it's manifold of intricacies can provide insights how isolated brain regions can function. 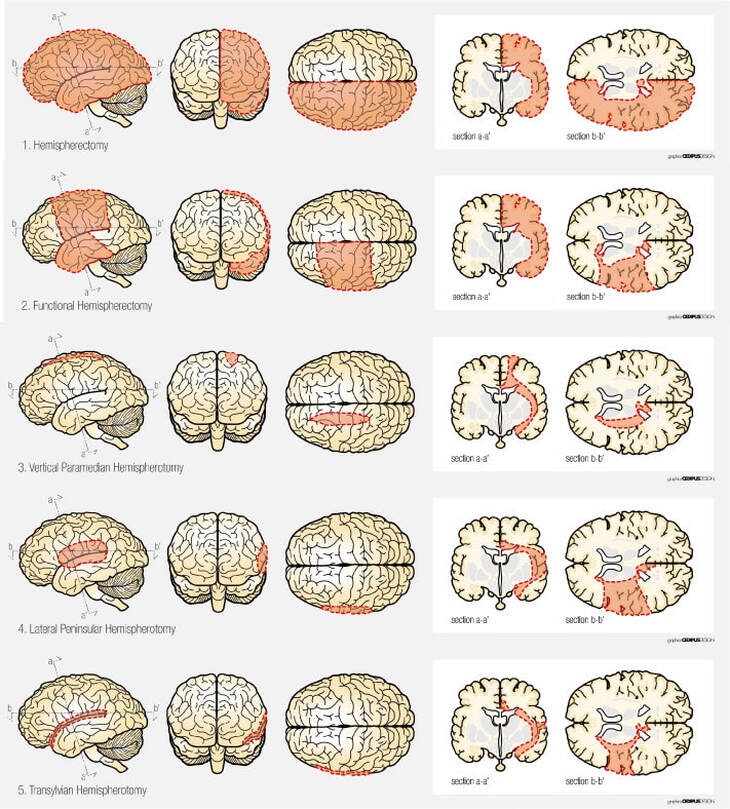 Figure 2: Schematic view of surgical techniques based on removal and/or disconnection. 1) (Anatomical) hemispherectomy, 2) functional hemispherectomy, 3) vertical hemispherotomy, 4) peri-insular hemispherotomy, 5) trans-sylvian functional hemispherectomy Picture from Marras, C.E et al. (2010). Hemispherotomy and functional hemispherectomy: Indications and outcomes. Epilepsy Research, 89(1), pp. 104-112
0 Comments
|
Proudly powered by Weebly
 RSS Feed
RSS Feed